
Almost half of the population of Australia suffer with at least one chronic disease and these conditions account for the vast majority of the causes of illness, disability and death. Chronic diseases are also on the rise in our society, mainly due to longer life expectancy & a historical change in lifestyle.
So what is a chronic disease?
A chronic disease is a medical condition that is long term and persisting, slow to progress but can lead to severe disability and a shorter lifespan.
Examples of chronic diseases that are common in Australia include:
- Diabetes Mellitus
- Heart disease
- Arthritis
- Asthma
- Chronic Obstructive Pulmonary Disease (COPD)
- Chronic kidney disease
- Chronic back pain
- Mental health conditions
- Some cancers
What can I do to help manage my chronic condition?
There are many complex factors that contribute towards disease such as genetics, gender & environment, yet many conditions are triggered by lifestyle factors such as smoking, high alcohol consumption, poor diet (and obesity) and lack of physical activity.
Make sure you have a great GP
When you go to see a great GP if you have multiple issues to discuss, they will break them down into what’s most important and start with those, and invite you to return to spend more time going through the rest of the things on your list. That’s because a great GP knows that rushing through everything in one go is not really doing justice to your needs. You can read more about what to look for in a great GP
Have a healthy lifestyle
Live a healthy lifestyle. Many people with chronic conditions feel better with a good diet, being as active as they can be, being a healthy weight, not smoking and minimising alcohol.
Medication
Understand the medication you take – make sure your GP reviews them on a yearly basis if you are taking them long term.
Management Plan
Ask your GP for a chronic disease management plan (see below)
The power of a good GP
People may not realise that GPs and practice nurses are experts in screening for risk factors of chronic health problems, poor lifestyle, recognise early symptoms as well as advising and empowering people on proactive lifestyle changes or active treatment to prevent the disease.
However, once a person has developed a chronic disease, the GP becomes the facilitator to direct that person’s care, with the focus being less on cure but control of progression, avoidance of complications such as disability, hospitalisation and early death.
It could be argued that good GP care in recent times has helped revolutionise the care of illness, with the realistic expectation for people to live a near normal life with a chronic disease rather than suffer significant suffering and an early demise.
What is an integrated chronic disease management plan?
The Australian Government continues to invest in GPs leading disease management through the chronic disease management plan (CDM), a medicare rebatable case meeting with the GP and/or practice nurse to work in partnership with the patient to set goals of treatment and plan how these are going to be reached. Goals usually have a pragmatic and realistic focus on achieving optimal health and functional outcomes in living with the condition. The plan will involve various measures that incorporates clinician-led medical treatment and lifestyle measures that the patient is given the responsibility to build into their routine.
Part of this plan often involves generating a team care arrangement (TCA) to enlist the help of 2 or more allied health professionals such as a physiotherapist, podiatrist, dietitian etc to reach these health goals. Up to 5 visits to private allied health professionals are subsidised per year under these plans.
Not everyone qualifies for a CDM & TCA plan; the rules stipulate that a person must possess a valid medicare card and have a chronic medical condition. Medicare have entrusted GPs with the discretion of what constitutes a chronic disease, yet it is essentially an illness that has lasted for at least 6 months.
Separate from the CDM, there are also separately funded GP-led care plans enabled for diabetes and mental health, two of the more common long term health problems in our society.
Chronic disease management with an independent GP who consults at HealthMint
The Independent GPs who consult at HealthMint agree that the value of a high quality plan comes in a skilled, perceptive and enthusiastic GP and/or practice nurse dedicating a good amount of time to the patient, considering a tailored plan to the individual and providing practical tips on how to achieve the best health outcomes.
The Independent GPs consulting at HealthMint are confident that they provide a superior service since time and effort have been put into gathering an excellent group of caring GPs and nurses who are provided with the time to spend getting to know their patients, enabling them to work in partnership to inspire and empower these patients to improve their health and quality of life in spite of their chronic disease.
The GPs recommend that if you find yourself hampered by unpleasant symptoms of a chronic medical illness on a daily basis then do not waste another day settling for second best, and book an appointment to discuss your management options.
You can also access the factsheet for patients on chronic disease management.


 2. Exercise assists in weight loss and helps prevent unhealthy weight gain
2. Exercise assists in weight loss and helps prevent unhealthy weight gain 3. Exercise reduces the risk of and helps to manage cardiovascular disease, reduce risk of heart attack, lower blood cholesterol, lower blood pressure
3. Exercise reduces the risk of and helps to manage cardiovascular disease, reduce risk of heart attack, lower blood cholesterol, lower blood pressure 4. Social interaction and exercise go hand-in-hand
4. Social interaction and exercise go hand-in-hand 5. Build strong muscles and bones
5. Build strong muscles and bones
 8. Lower the risk of falls with exercise
8. Lower the risk of falls with exercise
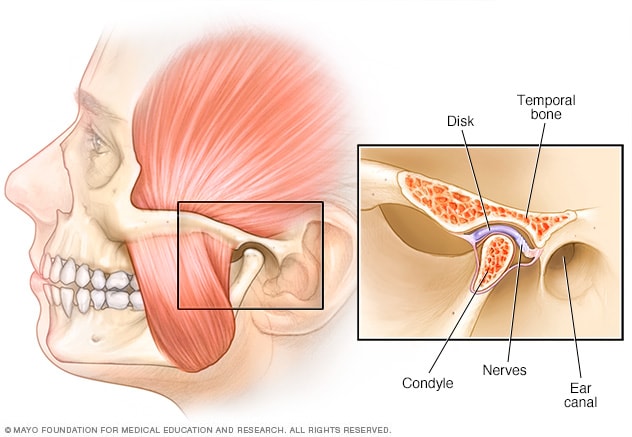
 What can cause TMJ pain?
What can cause TMJ pain? If you or someone you know may be suffering from any of the above signs of TMJ, you can
If you or someone you know may be suffering from any of the above signs of TMJ, you can 